An exciting new simulation-based education programme is getting rave reviews from our final year students on how it helps prepare them to step into the shoes of a junior doctor this summer.
FY1 PracTiSCE Week (Practical Training in a Simulated Clinical Environment) is run in the School’s state of the art simulation suites and presents students with real-life scenarios involving the latest VR technologies, high fidelity mannequins and simulated patient actors, all focused around three acutely ill patient journeys.
Helen Box is the School’s Director of Clinical Skills, Simulation and OSCE and led the development of FY1 PracTiSCE Week ready for launch this academic year.
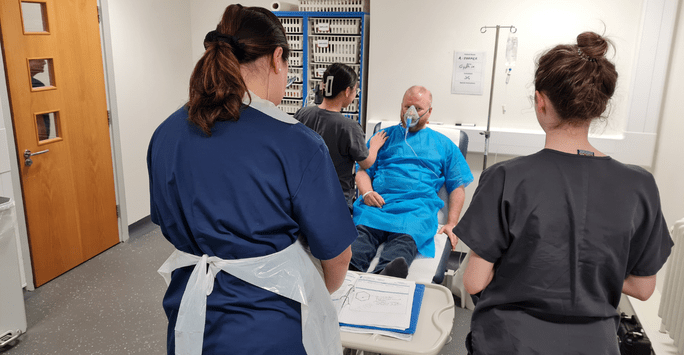
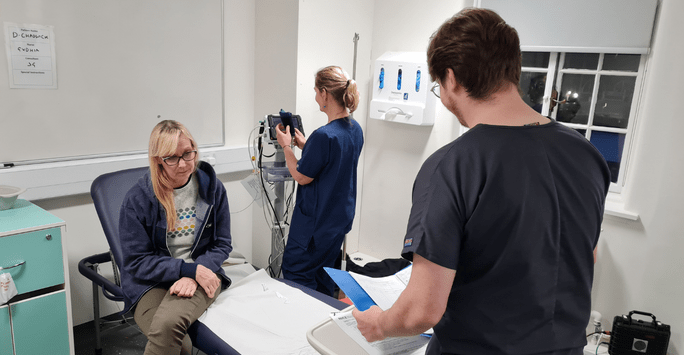 Student doctors take on a scenario during FY1 PractTiSCE Week
Student doctors take on a scenario during FY1 PractTiSCE Week
Helen says, “Changes to the Year 5 curriculum this year brought about an exciting opportunity to enhance our acute care teaching offer and allowed us to create an authentic and realistic simulation training week for our final year student doctors. The FY1 PracTiSCE week provides students with the opportunity to experience and rehearse the management of acutely ill patient scenarios in a safe and supportive environment to make mistakes and learn from them, and helps better prepare students for graduation and practice as a foundation trainee.”
The training programme is a stand-out addition to the School’s new MBChB Year 5 curriculum and builds on student feedback and learnings developed throughout the pandemic.
Professor John Ellershaw, Core Skills Supra-Theme Lead, explains, “As part of the region’s COVID-19 response, the School created the sub-FY1 role, allowing students in their final months of studies to step up and into the role of an FY1 doctor and provide crucial frontline support in patient care. Students fed back to us how useful this was in developing independence in their practice ahead of their official FY1 start and this has shaped major optimisations to our final year of training, including a six-week Pre-Foundation Apprenticeship (PFA) placement and a new week of simulated clinical training on campus.”
The Pre-Foundation Apprenticeship is a six-week placement that gives students the opportunity to work alongside foundation doctors and clinical teams and show progress towards independent practice and being able to work independently within the team at the level of a new F1 doctor.
FY1 PracTiSCE Week is scheduled earlier on in the academic year to help set students up for success later on. So, what does the week look like in practice?
The week begins with Day One set up to represent a long day on call running from 8.30 until 17.00. Students are introduced to the patients they will be caring for over the course of the week and rotate in small groups through a series of workshops ran in a simulated A&E environment where they build on skills in clinical reasoning, decision making, prescribing, prioritising and handover.
 The scenarios use a mix of actors and high fidelity mannequins
The scenarios use a mix of actors and high fidelity mannequins
Students then take on ‘SimCom’, a day of high-fidelity simulation training involving a series of Communication for Clinical Practice (CCP) workshops and immersive simulations where they practise the technical and non-technical skills needed to manage complex clinical situations.
Dr Isobel Jenkins is Year 5 Lead for CCP and was heavily involved in creating the SimCom portion of the programme, along with Mr Jeff Goulding, Lecturer in Simulation Based Education.
Dr Jenkins says, “This day really pulls together a lot of the core skills learning from previous years, including non-technical aspects around managing a team, judging a situation and self-awareness, i.e. how to manage your reactions to the complex, rapidly evolving immersive scenarios that you are presented with.
The simulation suite is set up as a functional hospital space containing patients, concerned relatives and the occasional overwhelmed team member, all played by actors and trained role players, out to create interruptions and distractions.
The aim is to provide the look and feel of a real-life hospital setting that is still a safe space for trial and error from the students before they experience this on the ward.
A key part of the day is a peer debrief which presents a fantastic opportunity for individual, focused feedback. Students are supported through this by a facilitator as well as their peers, who have been observing the scenarios via live stream and are ready to give feedback and help students work through their thoughts, emotions and behaviours related to the situations they faced, as well as explore challenges and test out concepts and theories.”
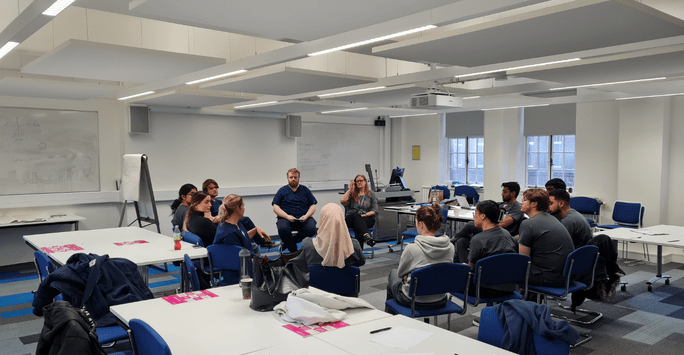 Students debrief after tackling a complex clinical scenario
Students debrief after tackling a complex clinical scenario
Another popular part of the programme is an introductory session in Procedural Ultrasound giving students plenty of hands-on practice in handling and adjusting an ultrasound probe, optimising an image, identifying common blood vessels and undertaking practical tasks.
The week concludes with a series of Safety and Error Recognition Workshops where students are joined by a group of final year student nurses to explore systems drivers for error, analyse critical incidents and consolidate and build upon understanding of clinical human factors.
Mr Goulding says this interprofessional learning has been a big hit with students.
“The immersive clinical scenarios the students take on really explore the impact of task overload and uncertainty on situational awareness. The nursing students are the first responders, and our student doctors respond to their call for help as FY1 doctors. They get to see how interruption and distraction impacts human performance, all while managing a deteriorating patient in an authentic clinical scenario.”
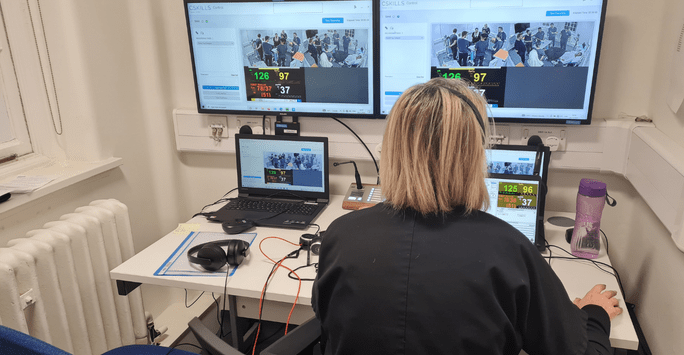 Observing a clinical scenario from the control room
Observing a clinical scenario from the control room
The work on Safety and Error Recognition includes a VR workshop, a new innovation in the curriculum for which the School has worked with the virtual engineering centre to create a virtual 3D 360-degree interactive representation of the simulation suite. This is populated with systems elements that could cause an accident. Students are tasked with navigating the environment using a PC or headset and compete in groups to find as many latent factors for error causation as possible – an aspect of the learning that has boosted energy, engagement and feedback and helps end the week on a high.
Mr Goulding has been delighted with some of the on-the-spot feedback the team have been receiving from students.
“What they’re coming away with is really what we set out to achieve. They are talking about the importance of handover, of knowing when to escalate and of getting a fresh perspective.”
The students are using the week to bring together many aspects of their training over the previous five years, including prioritisation, effective communication, escalation and professionalism.
This has been further underlined in student evaluations on the week as highlighted by Deputy Director of Clinical Skills Mrs Cathy Carr.
“We have been getting comments like, ‘I think this is the best week of uni I have had from an educational perspective, I found it really helpful how it was explicitly relevant to becoming an FY1.’ and ‘One of the best teaching weeks I have had at the university as it felt applicable and practical.’
Working with student nurses has stood out as a highlight of the week with students eager for more interprofessional learning, and they have appreciated both the ‘fun’ simulation sessions and being able to use ultrasound probes on each other.
With all sessions now complete, in March we will perform a full review of the programme, really drilling down into student feedback and data in order to develop the teaching further and create additional materials to support the students’ learning.”
 A student doctor interacts with a simulated patient actor
A student doctor interacts with a simulated patient actor
Professor Hazel Scott, Dean of Liverpool School of Medicine, has commended the team on a superbly put together, joined up piece of teaching. “Having decided it was important to do, the team worked tirelessly and against the clock to design and build a comprehensive programme in time for the start of Year 5. It is enhancing our Year Five students’ experience by enabling them to experience this learning ahead of their PFA placement later on in the year, where they can really rehearse their learnings before stepping into the FY1 role.”