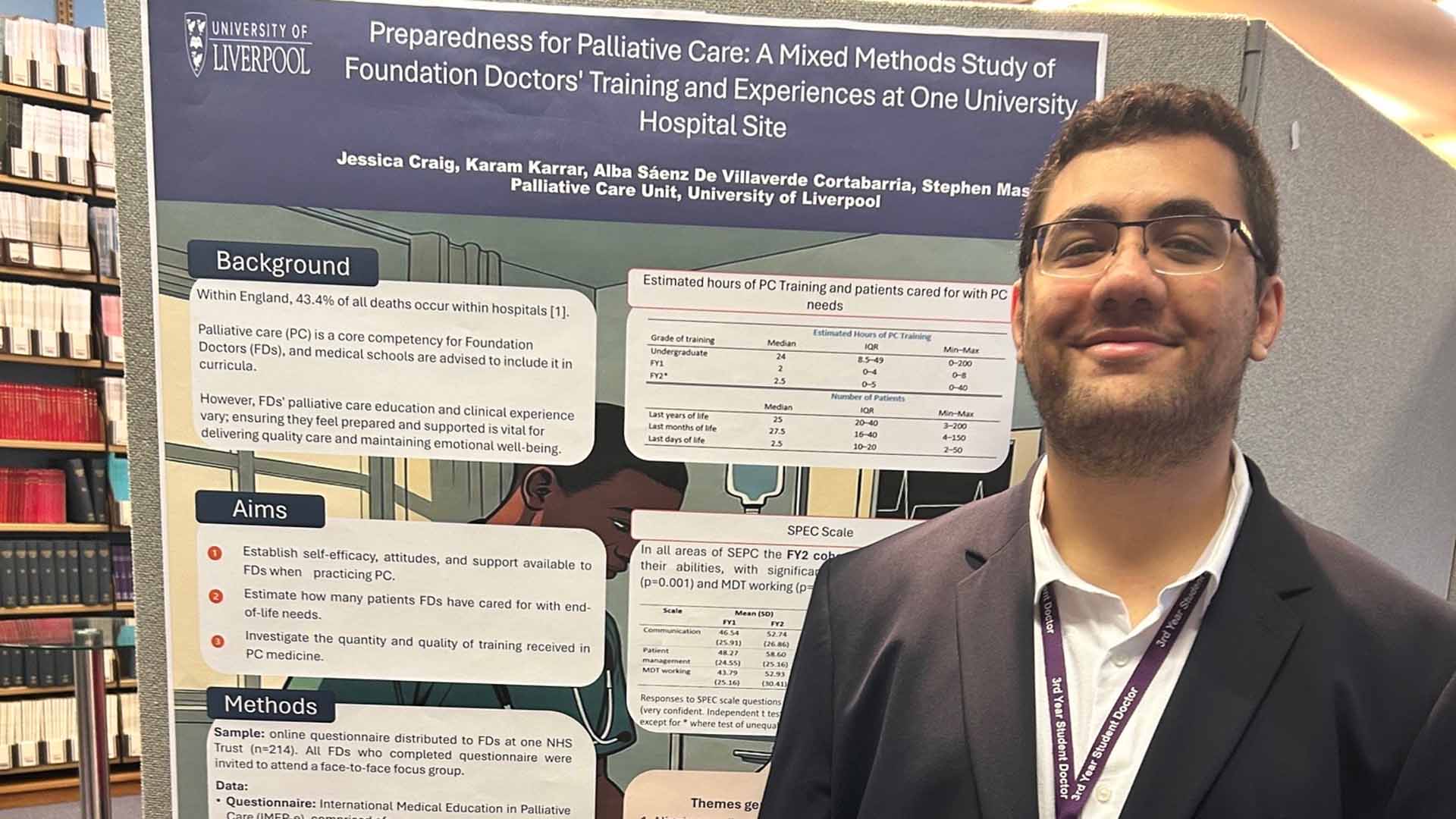
Year Three Student Doctor Karam Karrar recently had the opportunity to present his research into preparedness for Palliative Care amongst F1 and F2 doctors on behalf of the University of Liverpool’s Palliative Care Team at the annual Association for Palliative Medicine (APM) Undergraduate SIF national conference in London.
I began to enquire about any research projects that I could get involved with towards the end of first year and began working with PalPrep (the research group) from early second year. The project “Preparedness for Palliative Care: A Mixed Methods Study of Foundation Doctors' Training and Experiences at One University Hospital Site” was led by Dr Jess Craig and supported by Dr Stephen Mason from the Palliative Care Unit at the University of Liverpool.
We began by generating themes for qualitative data taken from focus groups with foundation doctors on experiences with formal and informal undergraduate palliative care teaching and seeing how confidence levels varied between the different medical schools the doctors graduated from.
We then analysed this data and looked for trends and correlations. Our main findings were that:
- Training in palliative care is inconsistent across the country;
- Confidence improves with progression through foundation training;
- A structured, nationally implemented palliative medicine curriculum at undergraduate and postgraduate levels is required to enhance foundation doctors' preparedness, improve patient care, and safeguard doctors' wellbeing.
We found that medical courses with established formal placements in palliative care environments (e.g. the 2-week hospice placement in fourth year at Liverpool) tended to have a higher value on the Self Efficacy in Palliative Care scale (SPEC). The study also showed that postgraduate, ad hoc (‘on the job’) learning accounted for a lot more understanding of palliative care teams than formal undergraduate teaching for a lot of medical school graduates, which is a little surprising.
There were limitations of course to the study, for example with the sample being from only one hospital site.
But I think the trend that most concerns me from the initial data is that a lot of training happens serendipitously, i.e. not standardised, meaning opportunities may be better for some students than others.
The conference itself covered many interesting topics from how palliative care is established and integrated into medical school curricula; to discussing and debating physician assisted suicide (PAS) and how this may be implemented into undergraduate education, as well as scope of practice as a foundation doctor.
A standout feature of the day was the creative use of technology and innovation in teaching, such as using AI to practice discussions around dying with a simulated patient, or using VR to practice consultations with SBA-style questions and personalised feedback included, or even using board games and escape rooms to teach palliative care to medical students!
Overall, it was an inspiring and educational day. I’m grateful to Dr Stephen Mason and Professor John Ellershaw for their support and for making this opportunity possible.
Discover more
- Learn more about how palliative care fits into the curriculum here at Liverpool on our A100 and A101 (graduate entry) programmes.
- See how the School can support your interests in clinical research on Student Research in the student intranet.