Every 24 March we commemorate World TB Day with the World Health Organisation. The theme for 2024 is ‘Yes! We can stop TB!’ and we wanted to update you on how we are playing our part in making that statement a reality.
What is World TB Day?
The World Health Organisation (WHO) chose 24 March as World tuberculosis (TB) Day as on this day in 1882 Dr Robert Koch identified the bacterium responsible for TB infection. This knowledge enabled the subsequent research that has led to successful treatments for this debilitating disease.
“Each year we commemorate World TB Day to raise public awareness about the devastating health, social and economic consequences of tuberculosis (TB) and to step up efforts to end the global TB epidemic.” - WHO
Why is understanding the impact of TB important?
While TB often starts its infection in the lungs, it can disseminate elsewhere in the body, such as the kidneys, the spine, etc. TB disproportionately impacts low- and middle- income countries (LMICs), who report the vast majority of the world’s diagnoses. WHO reported that around 10 million people become infected with TB each year and it was the second biggest infectious killer after COVID-19 in 2020.
Understanding the scale of a devastating disease is hard to comprehend, but the number of TB diagnoses and deaths is even more difficult to understand because it is treatable and preventable with the right medicines. There should be far fewer diagnoses and deaths than there are.
There are medicines that can treat TB and prevent infection, but they either aren’t reaching or aren’t optimally practical for those who need them most.
How does this connect to the LONGEVITY project?
The LONGEVITY project represents a consortium led by the Centre of Excellence for Long-acting Therapeutics (CELT) co-Director Prof. Andrew Owen and funded by Unitaid. One of our goals is to take drugs known to be effective and safe for use to treat or prevent TB, malaria and hepatitis c virus, and make them as convenient for patients as possible by creating long-acting medicines.
For example, currently available drugs used in TB prevention must be taken daily by mouth and missing a dose can impact how well it works. This can make consistent and sustained intake difficult for patients. By creating a long-acting medicine with these drugs, patients will only need one injection to maintain drug levels for several weeks. Teams within LONGEVITY are committed to creating a long-acting version of the drug and making sure that access to it is prioritised to LMICs.
An update of our long-acting rifapentine work we presented at CROI
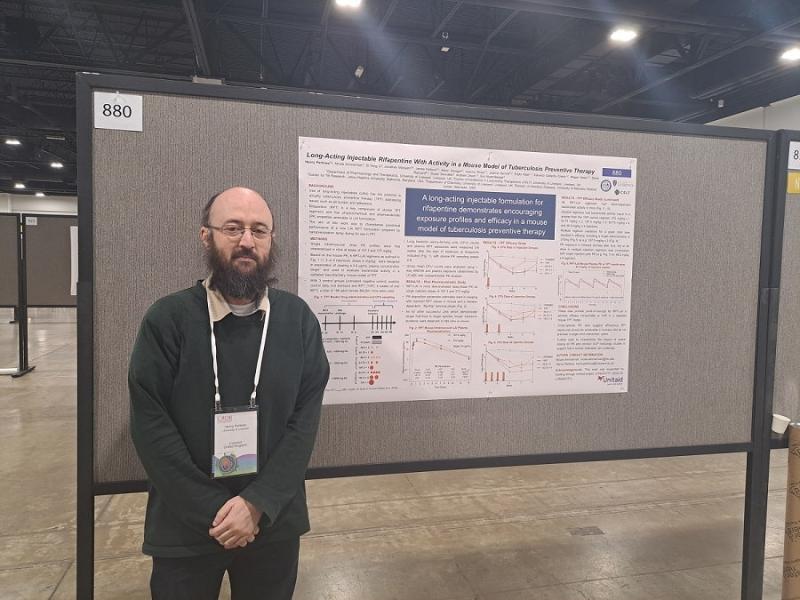
Dr Henry Pertinez is the co-author on an upcoming publication, headed by Dr Nicole Ammerman, that he presented at the 2024 Conference on Retroviruses and Opportunistic Infections (CROI) in Denver this month. Henry has been working at the University of Liverpool since 2012, starting here on a TB-related grant, and has worked with CELT as a lead pharmacometrician since our launch in 2020.
Being a pharmacometrician means analysing pharmacological data, which in CELT means Henry has been heavily involved in our important modelling work. Modelling within CELT is when we simulate tissues or whole people using mathematical methods combined with quantitative data we have about a drug to predict or explain what the levels of that drug will be in the body after a dose and how this will relate to how it will work. Modelling is paramount in our work as it means we avoid wasting time and limited research resources on trials with only a small chance of success.
Professor Eric Nuermberger, who is a Professor of Medicine at Johns Hopkins University School of Medicine (JHU) led the in vivo efficacy assessments for the CELT long-acting formulation. Johns Hopkins University are an important partner within the LONGEVITY project consortium. Among other research, Prof. Nuermberger researches TB and finding new ways to shorten the duration of TB therapy. The connected philosophies of his team’s work at JHU and LONGEVITY means collaboration aligns well, as exemplified by this poster and other collaborative outputs between JHU and CELT.
Henry’s poster showed people the supporting work for the technology between chemistry and pharmacology within LONGEVITY’s long-acting rifapentine project. A journey from the new formulation development (led by CELT co-Director, Prof. Steve Rannard), initial pharmacokinetic studies at CELT, Henry and the team’s modelling work, and Prof. Nuermberger’s in-vivo efficacy assessments. Henry’s modelling work meant we had an idea that the drug would behave how we expected it to before we trialled it in a living being.
The model looked at both the pharmacokinetics of the drug, i.e. the time course of the drug’s absorption, metabolism and removal from the body, and the pharmacodynamics, i.e. the effect of the drug will have on the body over that time course. Modelling means not only that we can have some understanding if a drug will work, but what concentration and timespan will produce the most effective use of it.
The poster shows that there is preclinical proof of concept for both pharmacokinetics and pharmacodynamics of this long-acting rifapentine medication. The drug behaved how we wanted it to and it worked the way we wanted it to. This proof of concept led the pathway for the next steps at Johns Hopkins University who could reduce the number of in-vivo trials by concentrating only on the formulation we knew had the best chance of success.
What are the next steps from proof of concept?
Henry’s modelling and Johns Hopkins’s work means we can now move to toxicological studies. We know rifapentine isn’t toxic at currently recommended doses as it’s already approved for use in patients, so this is just to make sure the new formulation of the drug is also not toxic. The collaborative work has been able to suggest an effective dosing regimen, so after toxicology we can look for manufacturing scale up to make enough drug to move onto clinical trials in humans.
As this work is on drugs that are already on the market in other formulated versions, because we know they work and are safe, the clinical trials will aim to confirm the long-acting medicine works as we would like it to in a humans.
Why is it important?
TB disease has such a huge impact on the world and its global inequity shows that having effective medication hasn’t been enough to eradicate it. A long-acting rifapentine is hoped to dramatically help our journey to ending the burden of this epidemic by making the TB preventative therapy easier to disseminate and administer. A long-acting medicine will require less visits to dispensaries and should avoid that difficulties that impact people’s ability to take medication daily.
Despite being preventable, and treatable if the disease does develop, 1.3 million people died from TB in 2022 and the majority were in LMICs. One of the four key messages of this year’s World TB Day is “tackling health inequities to ensure health for all”, which is why LONGEVITY does the work it does and are committed to always prioritising access to LMICs of any long-acting medications we create.
We created a video for World Tuberculosis Day last year where we spoke to Monica Subba about the experience of living with TB.
The LONGEVITY project aims to simplify TB preventative treatment and reduce the number of patients requiring complex therapies for active disease.
Find out more about the LONGEVITY project's work on TB
The LONGEVITY Project is funded by Unitaid


The project also involves critical partners and collaborators in the Clinton Health Access Initiative, Johns Hopkins University, Medicines Patent Pool, Tandem Nano Ltd., Treatment Action Group and the University of Nebraska Medical Center