I’m Elliot Croft, a PhD student based in the Department of Chemistry. I obtained an MChem degree in Medicinal Chemistry with Pharmacology at the University of Liverpool. During my undergraduate studies, I undertook research projects focusing on polymer synthesis and controlling the size of inorganic nanoparticles for targeted drug delivery. Now, my research focuses on the development of bespoke dissolvable microneedle arrays (DMNs) for the treatment of glaucoma which provide sustained drug delivery which cannot be achieved using the typical treatment method – eye drops.
Living with Glaucoma
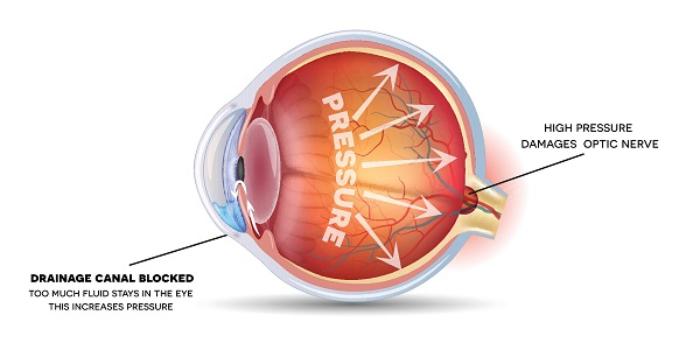 Glaucoma is the 2nd leading cause of irreversible blindness in the world. It is a lifelong condition affecting around 80 million people worldwide. Glaucoma relates to vision loss when the optic nerve (the nerve situated at the back of the eye which carries visual information from the eye to the brain) becomes damaged. This damage is usually caused by increased pressure within the eye (intraocular pressure or IOP). That's why early detection and treatment is so critical to preserve the visual function of the eye.
Glaucoma is the 2nd leading cause of irreversible blindness in the world. It is a lifelong condition affecting around 80 million people worldwide. Glaucoma relates to vision loss when the optic nerve (the nerve situated at the back of the eye which carries visual information from the eye to the brain) becomes damaged. This damage is usually caused by increased pressure within the eye (intraocular pressure or IOP). That's why early detection and treatment is so critical to preserve the visual function of the eye.
Treatment either involves surgery, which can be described as an extremely invasive approach with risks of infections, scarring and ultimately hypotony, or the use of pharmaceutical derivatives applied by a topical dose. There are many different classes of drugs to treat glaucoma, with the main objective to reduce the IOP within the eye and relieve the strain upon the optic nerve. Successful treatment can help slow or prevent further damage to the optic nerve, preserving vision for as long as possible.
Topical dosing however, is heavily limited by pre-corneal factors and the diversity of anatomical and physiological barriers within the cornea which leads to poor bioavailability of the drug. Therefore, patients require repetitive dosing regimens to sustain a therapeutic concentration, causing toxicity issues and poor adherence to prescribed dosages because of the extensive nature of their regimen. For a lifelong condition, this can be difficult to sustain and research has shown that over 90% are non-adherent with their prescription eye drops and almost 50% stop taking their medications before 6 months.[i]
Dissolvable Microneedle Arrays
The use of DMNs combines both the user-friendly nature of topical dosing but benefits from increased permeation through ocular tissue, linked to its needle-like shape, thus increasing the bioavailability of the active pharmaceutical ingredient for anterior drug delivery.
DMNs are fabricated from water soluble materials such as polymers. They can be applied to the eye to create transient micropores which allow the drug to bypass through hydrophilic and lipophilic layers of the cornea which alternative drug delivery systems, such as topical dosing struggle to permeate. They are described as minimally invasive due to their sub-micron size which prevents contact with the corneal endothelium, a barrier composed of a high concentrations of pain receptors within the eye.
One of the huge values of DMNs comes from their facility to prolong the therapeutic window, meaning treatments need to be administered far less frequently than topical doses, whilst achieving the same therapeutic effect. For example, a prescription of eye drops that require multiple applications daily could be replaced by DMNs that require administration far less frequently to deliver the required drug concentration over a period of weeks or months. This longer therapeutic window reduces issues associated drug accumulation, as well as improving patient adherence with the need for less dosing regimens.
A further advantage of DMNs have over topical dosing is the reduction of drug waste. Upon application, less of the drug is lost due to tear run-off so there is potential to decrease the amount of drug needed for application which could make it a more cost-effective method of drug delivery.
This research demonstrates the huge potential for DMNs to offer patients a revolutionary new glaucoma treatment option which is easier to maintain on an ongoing basis.
My Research Recognition
 For my research, I was recently awarded the 2022 Roy Mapstone Award for Ophthalmology and Vision Science Research. This is a prestigious award given to researchers who have demonstrated excellence within ophthalmology research.
For my research, I was recently awarded the 2022 Roy Mapstone Award for Ophthalmology and Vision Science Research. This is a prestigious award given to researchers who have demonstrated excellence within ophthalmology research.
I was also awarded runner-up prizes for the Chemistry Symposium Days in 2021 and 2022 as well as being awarded the best oral presentation for the 2021 Joint CDT/UKSB Future Leaders Conference.
As part of my studies, I have been lucky enough to be invited to present at prestigious events and conferences across the UK and Europe. Most recently in September 2022, I travelled to Bordeaux, France to attend the 32nd Annual Conference of the European Society for Biomaterials (ESB) where I presented a poster on my research. Click here to view my research poster.
[i] Nordstrom BL, Friedman DS, Mozaffari E, Quigley HA, Walker AM. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005;140(4):598-606.