Welcome to Liverpool: stay positive. stay brilliant. stay safe.
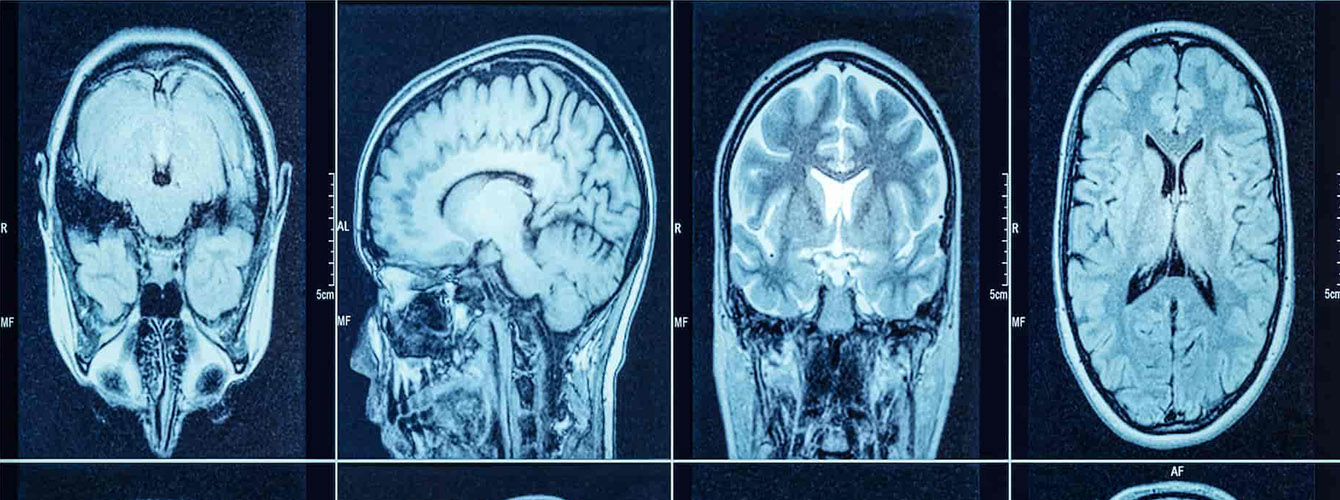
Improving the management of brain infections
The devastating impact of brain infections can be markedly reduced through prompt recognition, diagnosis and treatment. Research at the University of Liverpool has improved surveillance, diagnosis and management leading to new UK guidelines, with global impact. With close patient and public involvement, the Liverpool team increased awareness of brain infections, reaching millions through publications, courses and outreach events.
Patients are recognised, diagnosed and treated quicker, the median time to antiviral treatment for encephalitis in the UK fell from 48 hours to 10 hours leading to better outcomes, and saving up to an estimated £1,183,997,971 since 2013.
Background
Many brain infections are treatable. Yet brain infections such as meningitis (inflammation of the brain membranes) and encephalitis (inflammation of the brain itself) are a major emerging cause of disability and death.
Liverpool research aimed to understand the causes of this problem and improve practice through its NIHR-funded Brain Infections UK programme, delivered in collaboration with national hospitals, charities and the NHS, and the linked NIHR Brain Infections Global programme, delivered through international partnerships.
Research
The team examined treatment for encephalitis and meningitis nationally, through two major NIHR-funded programmes, Enceph-UK and UK-Meningitis, part of the Brain Infections UK portfolio. The former recruited 1,930 patients, the latter 1,870.
Misdiagnosis of encephalitis was common; 85% of cases showed subtle behavioural or personality changes which were often misinterpreted as psychiatric illness, rather than treatable brain infection. The Brain Infections Global Programme showed the importance of viral brain infections in Africa, and the role of emerging viruses on the brain including Zika, Ebola, Japanese encephalitis and in the UK, COVID-19.
Working in partnership
The team collaborated with Public Health England to examine trends in prevalence of both viral and bacterial brain infections in the UK. They showed that herpes simplex virus is the most common infectious cause of encephalitis, but that autoimmune encephalitis (caused by the body’s host defences) is growing in importance. The team showed viral meningitis is also increasing numerically in the UK and leads to a significant health economic burden.
The UK and international research was supported by an extensive patient and public involvement programme run through the NIHR Health Protection Research Unit in Emerging and Zoonotic Infections (Professor Tom Solomon is Director), working closely with the Encephalitis Society (Professor Solomon, Chair of the Society’s Scientific Advisory Panel 2010-2019, President since 2019; Dr Michael, Vice Chair 2019), and the Meningitis Research Foundation (Dr Kneen, Dr McGill and Dr Michael members of the Medical Advisory Group since 2015); this included joint grant applications with the patient and public involvement partners, co-delivery of the research, joint publications and shared dissemination events.
Impact
Liverpool research has greatly improved the likelihood that those suffering a brain infection, in the UK or further afield, will survive and avoid devastating disability. The impacts have been achieved through two main areas: firstly, improved awareness of brain infections among health care professionals and the public (vital to promoting early presentation and appropriate initial medical assessment); secondly, better hospital management (because correct and timely treatment has a dramatic effect on outcome).
Raising awareness to promote early presentation
In 2014 just 1 in 1,000 people had heard of encephalitis; by 2020, the figure was 1 in 5. Liverpool researchers drove this change through devising and supporting a plethora of innovative patient and public engagement initiatives.
Guidelines and their uptake
The group’s research resulted in the production of new national meningitis and encephalitis guidelines, which are now the primary reference point for all medical practitioners in the UK.
Impact through education
The guidelines feature heavily alongside other work from the team in the annual Liverpool Neurological Infectious Diseases Course (established in 2007), engaging 1,017 UK delegates (from 193 NHS Trusts) and 327 foreign delegates from 40 countries since 2013. 88% of respondents from the 2019 course agreed or strongly agreed that the course had informed their practice, with 71% recalling of one or more specific patients who had been helped.
Neurological COVID-19 Disease
The wider impact of the team’s research into recognising, diagnosing and managing neurological manifestations of infectious diseases is exemplified by their response to COVID-19. The team rapidly modified and distributed their standardised case definitions for neurological COVID-19 disease.
Improved health outcomes
The impact of the group’s work on improving management is best demonstrated by the case study of time to treatment for herpes simplex virus encephalitis with the antiviral drug aciclovir. Following the introduction of the national guidelines, and their implementation through the Enceph UK Programme, the median time to treatment dropped from 48 to 23 hours by 2013, and 10 hours by 2016.
Health economic implications
To calculate the benefits of this more rapid treatment, the team conducted a health economic evaluation. Initiation of treatment for herpes simplex virus encephalitis within 48 hours was associated with improvement in outcome, shorter hospital stays, and reduced total NHS costs per patient in the first year after diagnosis.