Why (and where) did mortality rates sharply rise in 2015?
One of the great public health successes globally throughout the 1900s (and beyond) has been the continual improvement in human longevity. In the space of 100 years, life expectancy for England and Wales improved from 51 (1910/12) to 79 (2010/12). Improvements in medicine, combined with better sanitation and standards of living, contributed to declines in mortality rates for all ages over this period.
In a paper published today here, we show how 2015 became the first year for nearly 50 years to experience a large spike in mortality rates. The graph below shows the relative change in mortality rates comparing the period July 2014 to June 2015 to the previous yearly period. Nearly all ages saw increases in mortality rates in 2014-15, with these increases largest among the elderly. We estimate that the period 2014-15 saw 39,074 extra deaths compared to if mortality rates had not changed.
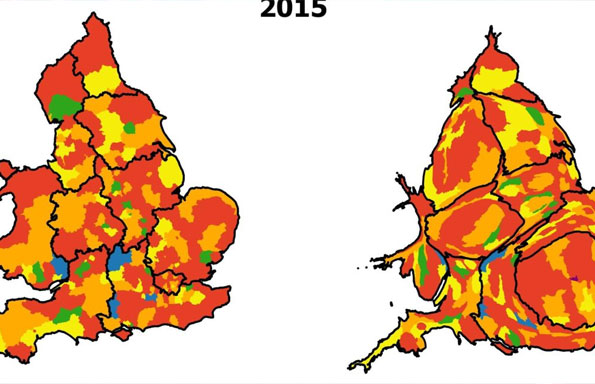
Where were these increases felt most? We focus only on the elderly (80+) who represent the majority of these deaths. Imagine taking every Local Authority District and then grouping them each into one of six categories based on the magnitude of their changes in mortality rates by age band (80-84, 85-89, and 90+, for males and females separately – so their changes for across a total of 6 groups). The maps below present the spatial distribution of the extent of these changes for the two time periods in question.
In 2013-14, we can see that few areas across England and Wales had experienced large annual increases in mortality rates. However, by 2014-15 we can see the spike in elderly mortality rates have occurred everywhere: in rich and poor areas, in urban and rural districts, in the North and South. The change between years is dramatic, and while 2013-14 was a good period with low mortality rates, what we see in 2014-15 is larger than any other year in the 21st century so far.
So what is driving these changes? Many of these deaths were due to increases in Dementia-related deaths, but we cannot be sure to what extent these increases were due to increased awareness of how to diagnose the condition. A flu epidemic would be the most obvious explanation, since this caused the last large spike in mortality rates in 1968. However, Public Health England described the influenza levels as only ‘moderate’ for the same period suggesting that it wasn’t the primary cause. Finally, it may be that we are starting to experience the effects of an ageing population, but if so then we would expect to see this more as a gradual effect instead of a sudden change (indeed the post-war baby boomers have yet to reach ages of 80+).
Rather, we believe that the rise in mortality rates reflects wider changes to our society. The lack of any geography suggests that any factor associated with the increase in mortality rates must be universal in their exposure. Cut backs to NHS funding and social care provision have placed pressures on the provision of health care, and issues such as delayed discharges or cancelled operations may have the largest ‘felt’ impact in the most frail of the population. These effects do not even have to be direct, but could also related to wider changes in social provisions (e.g. bus services being cut, ‘chit and chat’ groups disappearing, libraries being shut) which have accumulated in their ‘burden’. Could it be that the effects of austerity are beginning to materialize?
What is definite is that our findings demonstrate unprecedented changes in a time of no war, no great influenza epidemic, no freezing winter, and no cholera, with rising mortality rates among the elderly with no clear geographical pattern. Decades of progress in population health, with falling mortality rates becoming the norm, have been reversed, and the magnitude of this change suggests that 2015 is not an isolated event. Preliminary data show that mortality rates have remained just as high throughout 2016 and into 2017.
No matter the cause, it is clear that the ‘golden age’ of population health may be lost at least for now.